Obesity and associated lifestyle diseases are not restricted to the developed world. In fact, a growing number of emerging economies are finding that as obesity rises, so too do preventable conditions such as diabetes, hypertension, coronary heart disease and stroke. In South Africa, around one in four adults are obese, according to media fact-checking organisation Africa Check and the World Health Organisation. According to the WHO, 13% of adults globally were classified as obese in 2014.
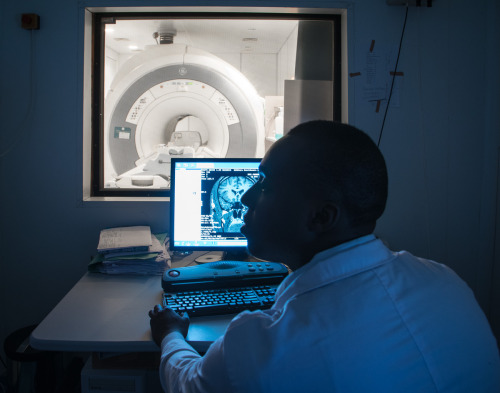
Measuring body-fat percentage is an important way to monitor and manage obesity and related illness, but accurately calculating body fat percentages is surprisingly difficult. With the recent installation of its bone densitometry system in South Africa, GE Healthcare is making muscle and fat measurement a lot easier. The technology identifies exactly how much muscle and fat is in the body and where it is located, helping doctors and their patients easily target zones for weight loss, advise on lifestyle changes and plan customised exercise routines, explains Tessica Chetty, an advanced applications specialist for GE Healthcare.
The same technology can also be used in osteoporosis management, as it assesses bone strength and can predict the likelihood of bone fractures.
In body-building competitions, the fat-to-muscle ratio is of utmost importance. Recently, the Worcestor Mediclinic, in South Africa’s Western Cape province, worked with a body builder to calculate her body-fat percentage using the bone densitometry system, providing valuable data to prepare her for competitions. Even her left and right arms were compared to determine minute differences in muscle and fat, with the results determining final preparations for competition.
Deidre Laing, a radiographer at Worcester Radiology, says she decided to work with the body builder in order to better understand the machine’s capabilities.
The bone densitometry system is also useful for non-bodybuilders. Laing has used the same technology to track changes in body fat percentages over time in a single patient. During the study, an initial scan was taken prior to any diet or exercise interventions. Following this, the patient went on a diet, after which the scan was repeated. She continued with the diet and added an exercise plan drawn up by a biokineticist based on problem areas highlighted on the scan. A third scan was able to show marked improvement after these interventions.
“You can actually see how you’re losing weight,” she says. As a result, patients are far more motivated to make healthier lifestyle choices.
Bone densitometry, like other medical scanning technology, empowers both patients and doctors with information they need to make informed decisions on treatment and diagnosis based on facts rather than guesswork. Now that we increasingly recognise the role of lifestyle decisions in maintaining good health, personalised healthcare information is set to become even more important.










